PNSD are pathological conditions of the peripheral nerves—comprising nerve roots, ganglia, plexi, and autonomic, sensory, and motor neurons—beyond the brain and spinal cord. These disorders precipitate lower motor neuron dysfunction, which manifests as muscle weakness and paralysis, or impair sensory neurons, causing abnormal sensations or sensory loss. As significant contributors to global morbidity, PNSD include a diverse array of disease types. Notably, peripheral neuropathy manifests a prevalence of 2.4% within the general population, escalating to 8% in individuals aged over 55 (1). The large economic burden of PNSD is pronounced, including direct healthcare costs and indirect costs incurred from productivity loss (2). Despite this, therapeutic strategies are largely palliative rather than curative. Neuropathic pain, a prevalent and debilitating symptom, remains difficult to manage, with pharmacological interventions offering only transient relief and carrying significant long-term risks. Current clinical guidelines thus prioritize non-pharmacological interventions, recognized for their efficacy and potential as alternative treatments (3, 4).
Given these challenges in managing PNSD, this study explored acupuncture, a non-pharmacological approach that has gained international endorsement, as a potential alternative. Acupuncture, a traditional Chinese medical practice, is now widely acknowledged in global healthcare and scientific research communities (5). This modality is effectively employed to manage a variety of conditions including chronic pain, osteoarthritis, seasonal allergic rhinitis, insomnia, and chronic functional constipation, demonstrating substantial therapeutic outcomes (6–10).
Recent years have witnessed a surge in international interest and research into acupuncture, particularly concerning its mechanisms and applications in PNSD. The literature consistently reported on the treatment’s efficacy and safety in managing diverse PNSD conditions such as diabetic peripheral neuropathy, cancer-related symptoms, neuralgia, and herpes zoster (11–14). Despite this, the existing literature remains eclectic and lacks systematic organization. Consequently, our study undertook a bibliometric analysis to map current research trends and identify focal areas within the field.
Bibliometrics, an interdisciplinary field, harnesses quantitative techniques to scrutinize published literature and documents through robust mathematical and statistical methods (15). This methodology merges mathematics, statistics, and philology, underscoring the importance of quantitative analysis (16). Among the plethora of tools available, CiteSpace is extensively employed for bibliometric visualizations, conducting co-citation and co-occurrence analyses.
This study aims to map the current landscape of references in acupuncture therapy for PNSD over the past two decades. It scrutinizes publication years, geographic origins, journals, research domains, contributing authors, prevalent keywords, and employs bibliometric techniques to explore hot topics and emerging trends. The review critically examines the evidence in the published literature regarding the safety and efficacy of acupuncture for PNSD and associated symptoms, comparing it to sham acupuncture or conventional medical therapy. Additionally, the effectiveness of acupuncture across various neuropathic conditions is assessed, where evidence allows.
2 MethodsThis study adheres to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and AMSTAR (A Measurement Tool to Assess Systematic Reviews) guidelines.
2.1 Data sources and search strategyData were sourced from the WoSCC on March 1, 2024, encompassing the Science Citation Index Expanded (SCI-EXPANDED), Current Chemical Reactions (CCR-EXPANDED), and Index Chemicus (IC). The investigation utilized search terms “Peripheral Nervous System Diseases” and “Acupuncture Therapy” over the period from January 1, 2004, to December 31, 2023. This search was restricted to English-language articles and reviews. Duplicates were systematically removed. Detailed methodologies, the screening process and the corresponding results are documented in Figure 1 and Supplementary Table S1.
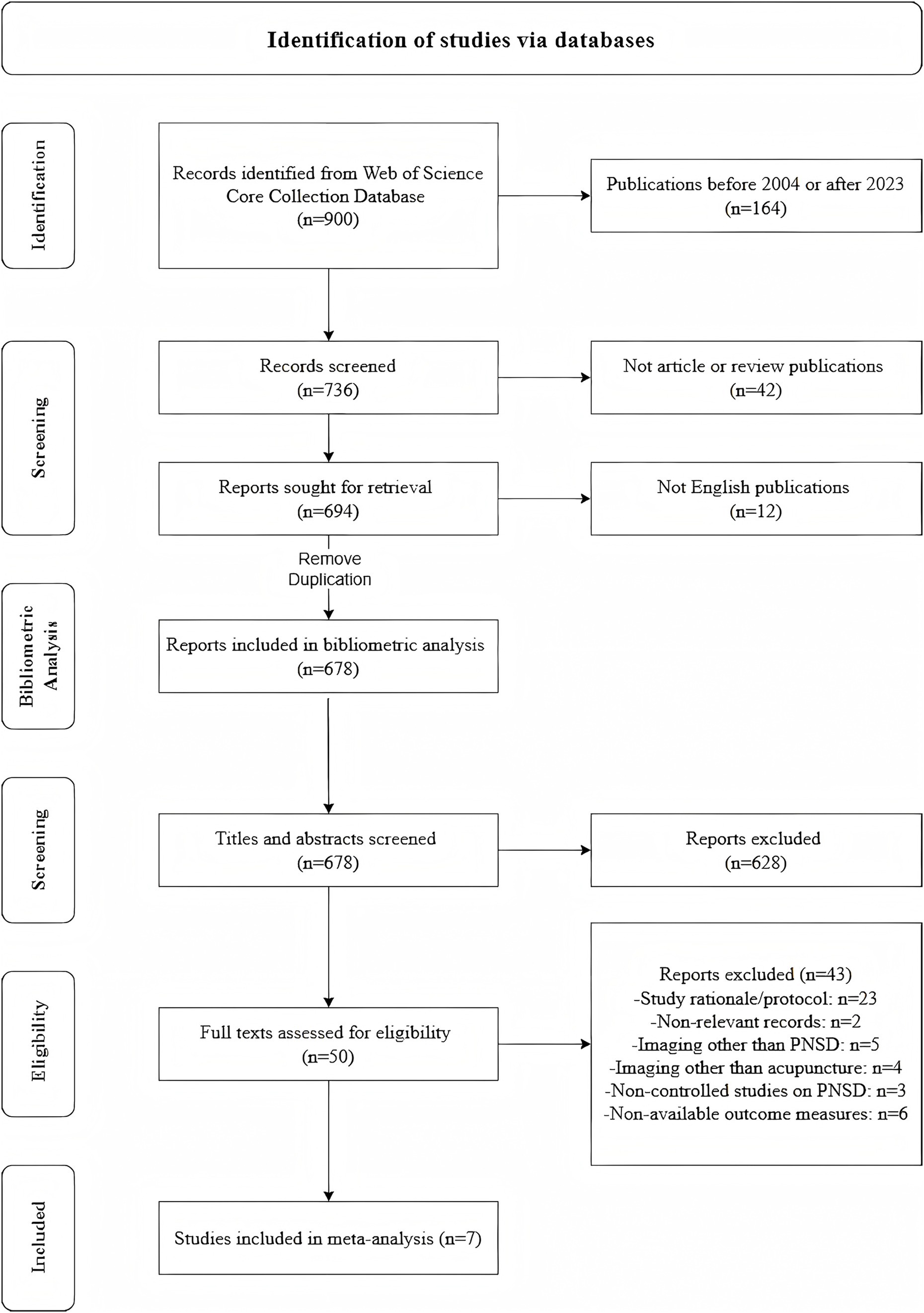
Figure 1. Schematic of data collection and screening.
2.2 Data extraction and visualizationIn this study, we utilized CiteSpace 6.1.R6 to construct a knowledge network map and conducted statistical analysis using Microsoft Excel 2021. Besides, SCImago Graphica (v.1.0.44) was used to analyze countries/regions, institution clustering, and published journals. The CiteSpace configuration was set to analyze data from 2004 to 2023 with a granularity of factor k = 25 and applied Pathfinder pruning to both sliced and merged networks. Nodes in the map represented unique units, with their size indicating occurrence frequency. Nodes exhibiting large dimensions and warm colors highlighted recent frequency surges, whereas those with purple perimeters signaled literature with notable centrality. Line thickness between nodes directly correlated with the level of collaboration or co-occurrence.
2.3 Inclusion and exclusion criteria for meta-analysis 2.3.1 Inclusion criteria1. Studies must be randomized controlled trials (RCTs).
2. Outcomes must include, but are not limited to, measures such as the Symptom Severity Score, Visual Analogue Scale (VAS), Global Symptom Score, or McGill Pain Questionnaire, or employ rigorously defined, study-specific objective criteria to differentiate responders from non-responders.
2.3.2 Exclusion criteria1. Non-primary research formats, including reviews, conference abstracts, letters, and experimental registrations, are excluded.
2. Non-randomized trials are ineligible.
3. Studies where data are non-extractable or presented in incompatible formats are not considered.
2.4 Study quality assessment in meta-analysisDuring the meta-analysis of included RCTs, we evaluated the quality of the RCTs using the Cochrane Risk of Bias (ROB) tool, which assesses random sequence generation, allocation concealment, participant and personnel blinding, outcome assessment blinding, incomplete outcome data, selective reporting, and publication bias. Disagreements were resolved through discussion or, if necessary, by consulting a third author.
2.5 Statistical analysisThe meta-analysis was performed using Review Manager 5.3. Risk ratios (RR) with 95% confidence intervals (CI) were calculated for dichotomous variables, while mean differences (MD) or standardized mean differences (SMD) were used for continuous variables. Heterogeneity was assessed via the chi-square test and quantified using the I2 statistic. A fixed-effects model was applied when I2 ≤ 50%, whereas a random-effects model was adopted for higher heterogeneity. Sensitivity analyses were conducted to explore potential sources of heterogeneity when substantial variation was detected. Statistical significance was defined as p < 0.05.
3 Results 3.1 Bibliometric analysis 3.1.1 Annual publicationsA total of 678 publications were analyzed in this study. Figure 2 depicts a clear upward trajectory in annual publication volume. Initial output between 2004 and 2010 remained at a low level, with annual totals not surpassing 20. A gradual increase was observed from 2011 to 2015, yet the pace of growth was minimal. A marked and continuous escalation in publication numbers commenced in 2016, and culminated in 90 articles, which constituted 13.2% of the total, in 2023. Additionally, we present the Times Cited status for the relevant research. The peak in Times Cited occurred in 2023, with the highest count reaching N = 2,603.
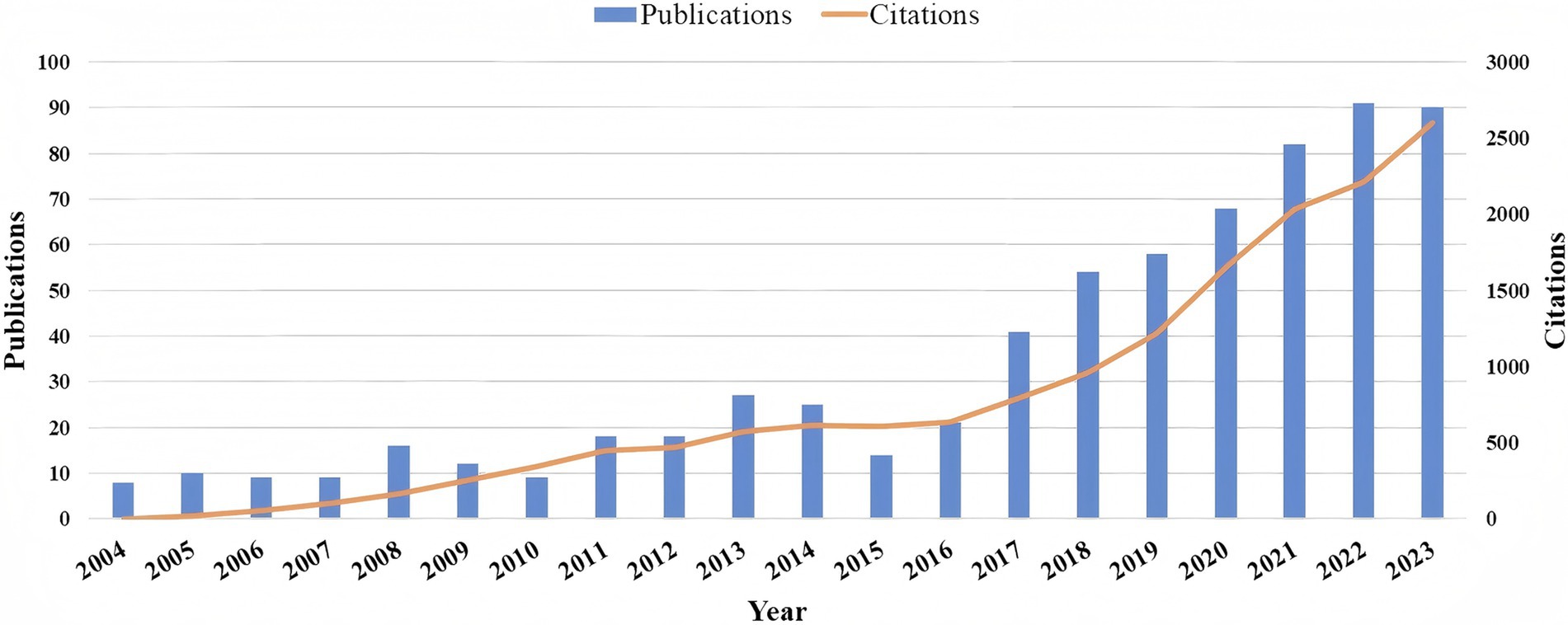
Figure 2. Timeline of publications and citations.
3.1.2 CountriesFrom 2004 through 2023, 41 nations have substantially advanced this area of research, as detailed in Figure 3 and Supplementary Table S2. The countries with the highest publication output included China (355 publications), the United States (160), South Korea (74), England (28), and Canada (22). In terms of centrality, England led with a score of 0.53, followed by Italy (0.38) and Sweden (0.37). Supplementary Figure S1 depicts the cooperative relationships among relevant countries globally, organized into four distinct clusters. Notably, the partnership between China and the USA stands out. The relatively dispersed nature of cooperation among the countries suggests a low level of overall collaborative engagement.

Figure 3. Distribution of countries.
3.1.3 InstitutionsFigure 4 and Supplementary Table S3 show that 439 institutions have actively contributed to this research domain. Leading the publication count were Kyung Hee University, China Academy of Chinese Medical Sciences, and Zhejiang Chinese Medical University, with 40, 30, and 28 publications, respectively. In terms of centrality, the University of Texas MD Anderson Cancer Center, Nanjing University of Chinese Medicine, and Fudan University stood out, each demonstrating significant network centrality values of 0.19, 0.18, and 0.18, respectively. Supplementary Figure S2 presents a network visualization of the cluster analysis for these institutions. The institutions are categorized into 5 cooperative clusters, demonstrating close cooperation among the organizations within each cluster and significant inter-cluster collaboration as well.
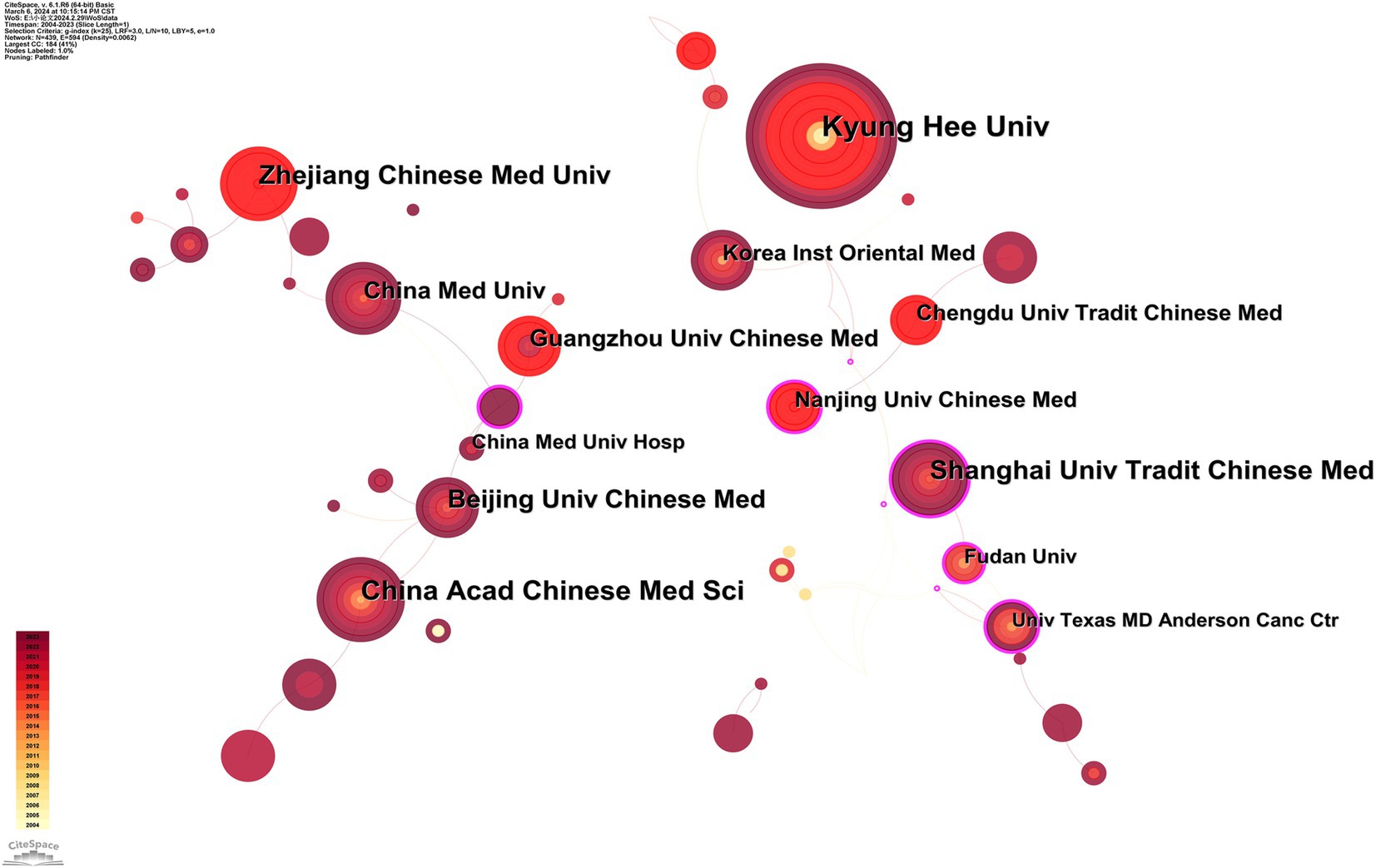
Figure 4. Collaborative map of institutions.
3.1.4 AuthorsIn the analysis of acupuncture therapy for PNSD, our study identified 605 researchers, of whom 5 has authored more than five publications, as detailed in Figure 5 and Supplementary Table S4. The size of the nodes in the network analysis corresponds to each author’s publication output. Fang Jianqiao (15) and Bao Ting (10), were identified as the leaders in this field. They were closely followed by Kim Sun Kwang (7), Eran Ben-arye (6), and Liang Yi (5). The data further reveal a distinct lack of collaborative efforts among these key figures. As leading scholars, Fang Jianqiao and Bao Ting have extensively evaluated the analgesic potential of acupuncture through RCTs, to compare its efficacy against placebo interventions like sham acupuncture or conventional therapies, as documented in references. Additionally, both researchers have explored the influence of patient expectations on the therapeutic effectiveness of acupuncture, proposing that psychological factors significantly contribute to treatment outcomes (17, 18). Specifically, Fang Jianqiao has concentrated on neuropathic pain disorders, including complex regional pain syndrome type-I and trigeminal neuralgia (TN) (19, 20). In contrast, Bao Ting has focused on the role of acupuncture in mitigating symptoms of chemotherapy-induced peripheral neuropathy (CIPN) and integrating complementary treatments to enhance the quality of life for cancer patients (21).
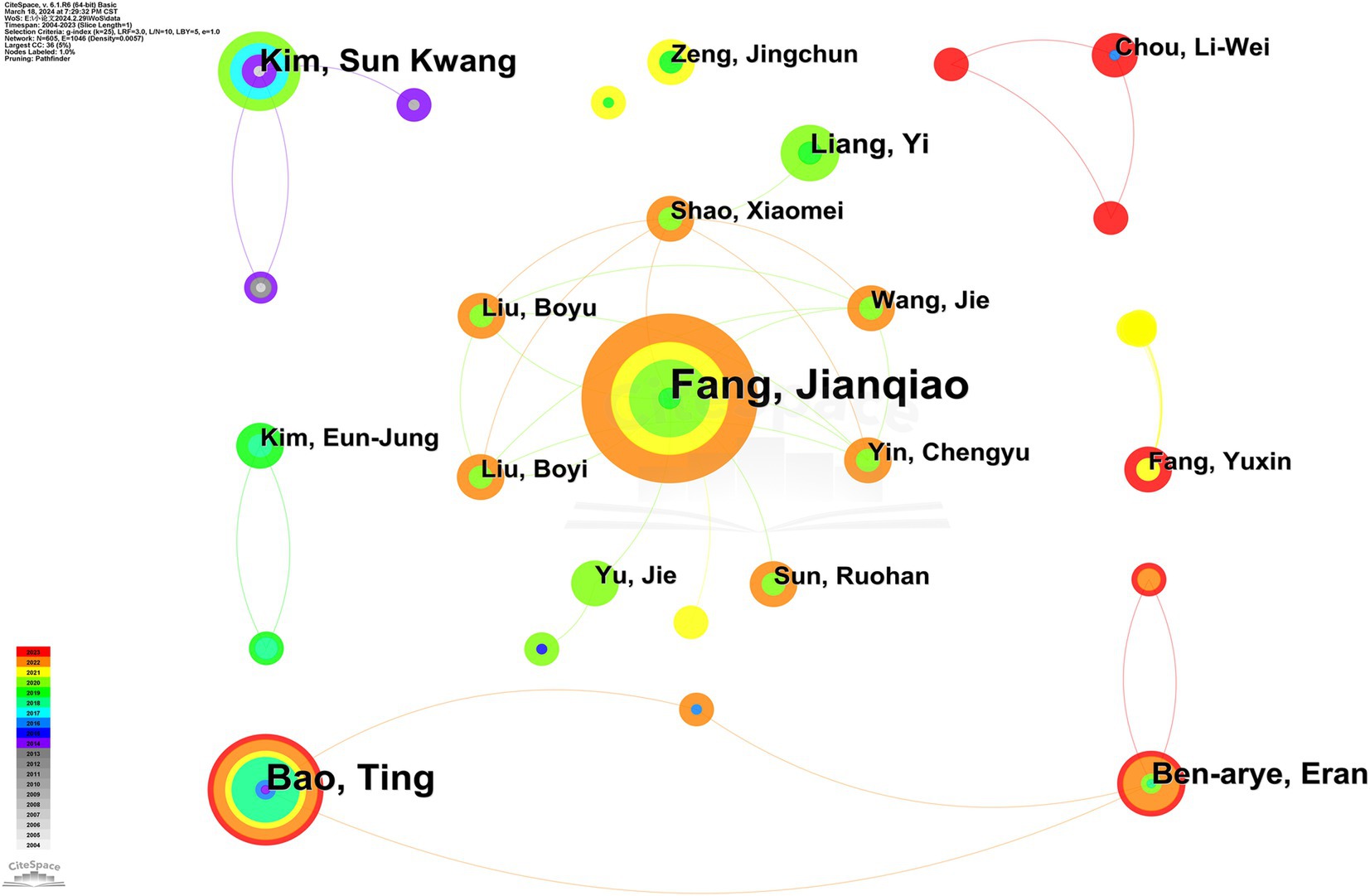
Figure 5. Collaborative map of authors.
3.1.5 JournalsResearch on acupuncture therapy for PNSD was broadly disseminated, with 277 journals having published on the topic. Supplementary Table S5 delineates the leading academic journals in this arena. “Medicine” emerged as the foremost publisher with 55 articles, followed by “Evidence-Based Complementary and Alternative Medicine (26),” “Acupuncture in Medicine (22),” “Journal of Pain Research (20),” and “Frontiers in Neurology (14).”
Supplementary Table S6 lists the top 5 cited journals in the study of acupuncture therapy for PNSD. Notably, “Pain” led with 386 citations, while “Anesthesia and Analgesia” was distinguished by its centrality, measuring 0.18. These findings underscored the significant influence and exemplarity of the articles published in these journals within the field.
In this study, CiteSpace was employed to construct a dual-map overlay, elucidating the citation relationships between journals as depicted in Figure 6. The left portion of the overlay maps the citing journals, whereas the right details the cited ones. Notably, the yellow trajectory reveals that articles within “Molecular Biology, Genetics” frequently receive citations from researchers in “Molecular, Biology, Immunology.” Additionally, the green trajectories demonstrate that manuscripts in “Medicine, Medical, Clinical” predominantly reference works across “Molecular, Biology, Genetics,” “Health, Nursing, Medicine,” and “Psychology, Education, Social.” Furthermore, the pink trajectories indicate that outputs in “Molecular, Biology, Genetics” and “Health, Nursing, Medicine” often serve as citation sources for publications in “Neurology, Sports, Ophthalmology.”
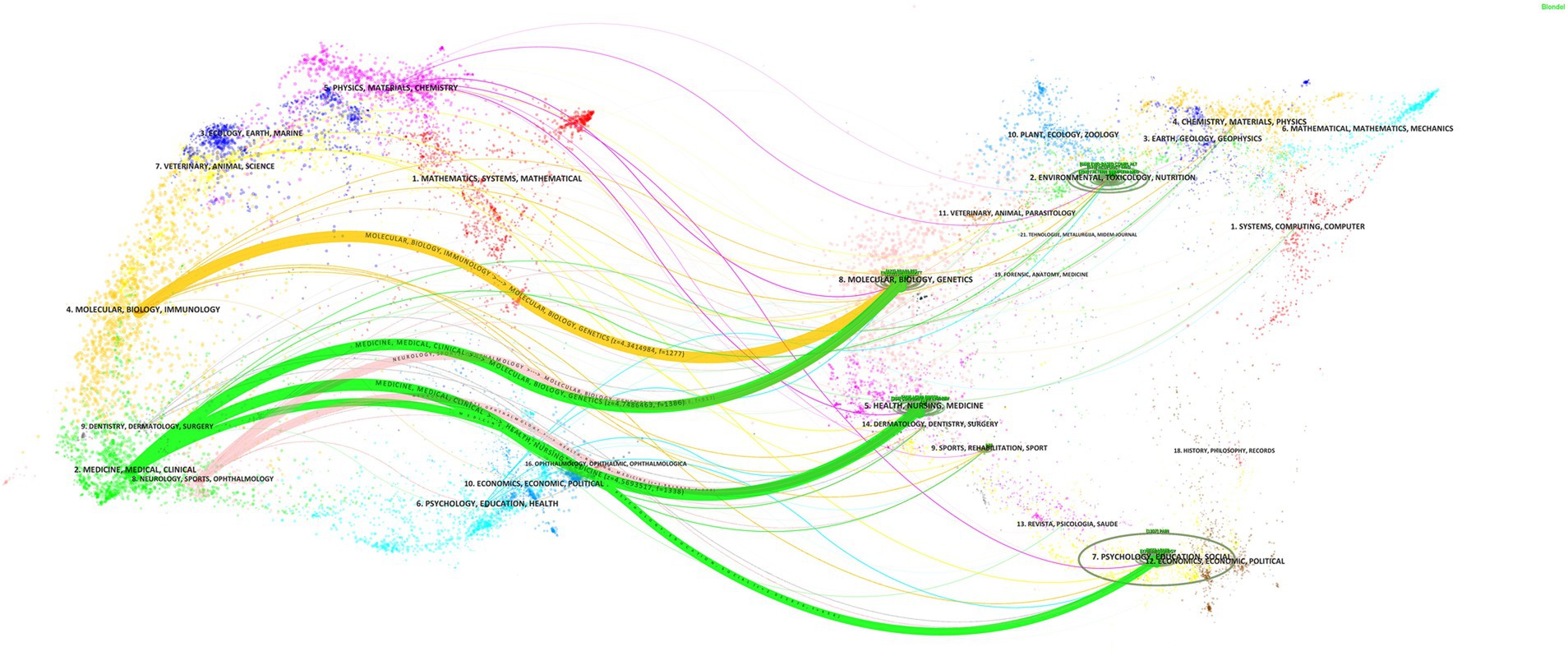
Figure 6. Dual-map overlay of journals.
3.1.6 Co-cited referencesReference co-citation, the concurrent citation of two or more papers by one or more subsequent publications, serves as a metric to assess the interrelationship among these documents. This measure generally reflects a strong linkage between the cited studies and the corresponding research fields, suggesting that the referenced works are typically of high quality and exert a significant influence within their respective domains. Table 1 list the top five references in terms of co-citation frequency. The study published by Lu Weidong (22) publication had the highest number of co-citations, with Alexandra Dimitrova (23) and Han Xiaoyan (24) works following closely (22).
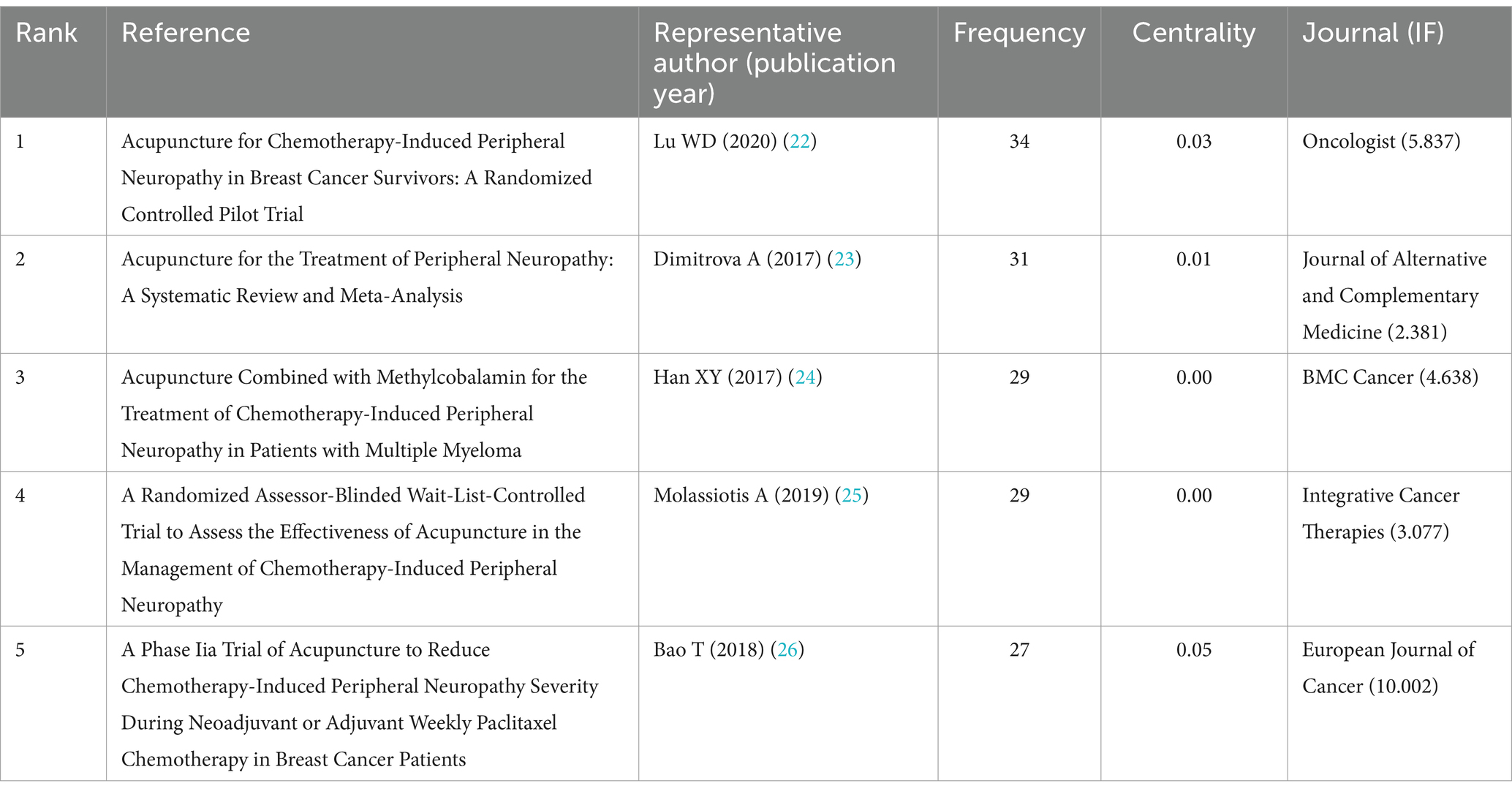
Table 1. The top 5 frequency of citations related to acupuncture therapy for PNSD from 2004 to 2023.
In this trial, Lu Weidong provided robust clinical evidence affirming acupuncture’s effectiveness, safety, and practicability in mitigating symptoms of CIPN. Notably, the study also highlighted acupuncture’s role in not only improving physical neuropathic symptoms but also enhancing survivors’ overall quality of life and functional status.
In a comprehensive meta-analysis conducted by Dimitrova (23), the therapeutic potential of acupuncture for treating peripheral neuropathy across various etiologies was evaluated. This study distinguished between neuropathy types and performing detailed individual subject analyses on conditions such as diabetic neuropathy and Bell’s palsy. The results indicated a significant variability in acupuncture’s effectiveness, contingent upon the neuropathy’s etiological basis.
In a 2017 publication, Han Xiaoyan revealed that acupuncture, used alongside methylcobalamin, could significantly improves outcomes for CIPN in multiple myeloma patients, thereby facilitating the integration of complementary therapies within conventional medical regimes (24). Alexander Molassiotis conducted a RCT in 2019 to underscore acupuncture not merely as a palliative intervention for pain but as a viable treatment strategy for CIPN. His research extended into examining the enduring effects of acupuncture through a methodologically robust, RCT incorporating detailed patient-reported and clinically validated outcome measures (25). A single-arm clinical trial published in 2018 by Bao Ting introduced novel perspectives on the prophylactic potential of acupuncture in managing CIPN, advocating for its use beyond therapeutic applications (26).
Citation burst, defined as a substantial increase in citations within a limited timeframe, serves as an indicator of emerging research focal points and potential future directions in a field. Figure 7A displays the five most prominent references exhibiting strong citation bursts, two of which are also among the most frequently co-cited works. Notably, Sven Schroeder et al. (77) had recorded the highest burst strength at 10.63. Moreover, Lu Weidong (22) had attracted considerable attention from the academic community since 2021, a trend that remains ongoing.
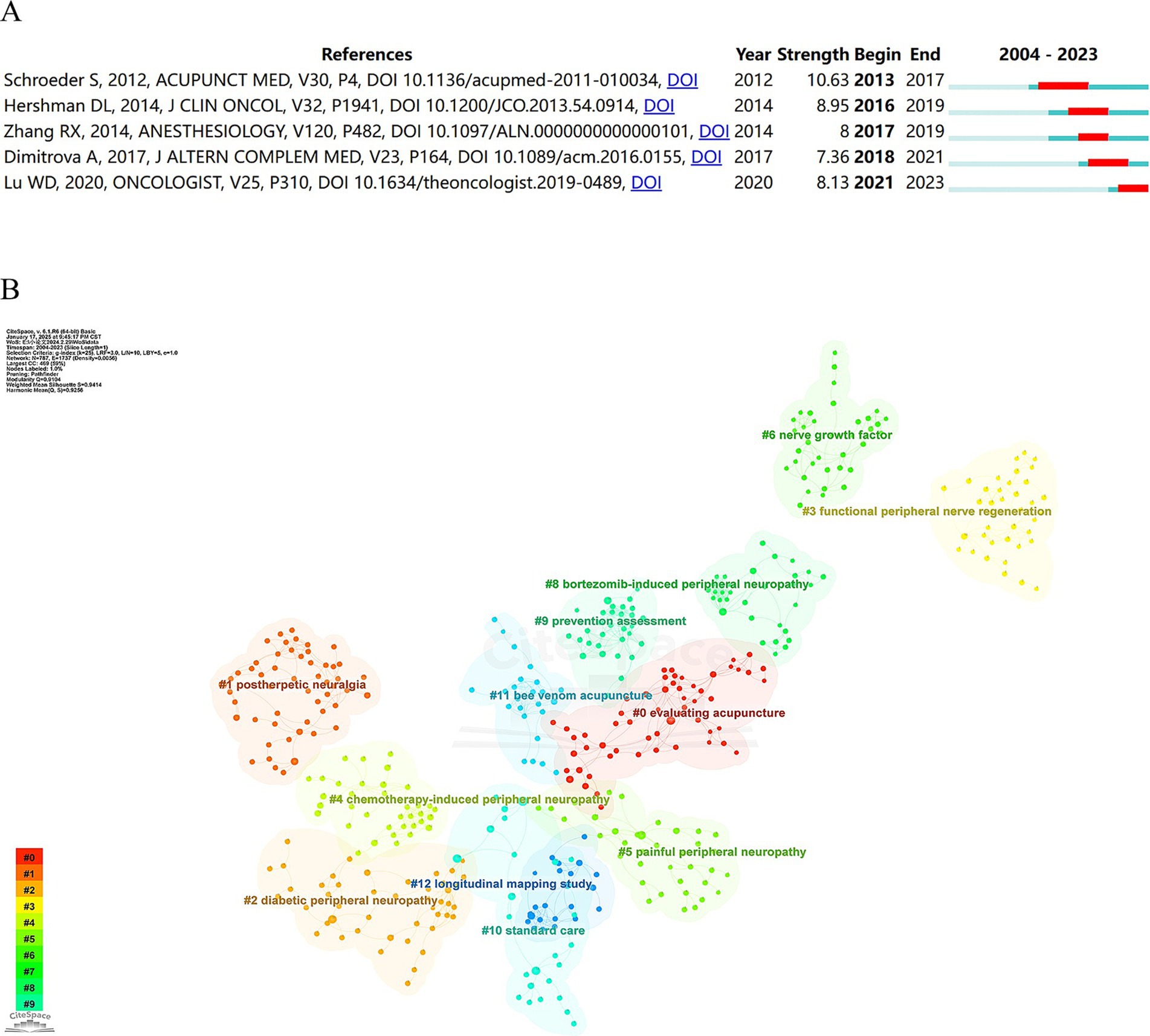
Figure 7. (A) Top 5 references with the strongest citation bursts. (B) Cluster map of co-cited references.
To elucidate the structure within the cited reference network, the log-likelihood ratio test (LLR) was utilized to identify clusters based on the keywords from the literature. This approach identified 26 distinct clusters (Figure 7B). Each cluster demonstrated a modularity score of 0.9104 and an average silhouette score of 0.9414, confirming the robustness and high resolution of the cluster graph. Analysis of the timeline view (Supplementary Figure S3) revealed that the primary research areas—namely cluster #1 postherpetic neuralgia (PHN) and cluster #4 CIPN —have emerged as recent research priorities, potentially indicating directions for future investigations.
3.1.7 KeywordsInvestigations into prevailing trends and focal points within specific disciplines often rely on the analysis of keywords marked by pronounced centrality and frequency. Supplementary Figure S4 depicts a map of keyword co-occurrence, and Table 2 details the principal keywords according to their frequency and centrality. In the realm of acupuncture therapy for PNSD, the past two decades have seen a consistent prominence of keywords such as “acupuncture,” “pain,” “management,” “neuropathic pain,” and “electroacupuncture (EA).” Keywords with the highest centrality, indicative of their pivotal role in the field, included “acupoint stimulation,” “activation,” “peripheral nerve injury,” “allodynia,” and “electrical nerve stimulation.”
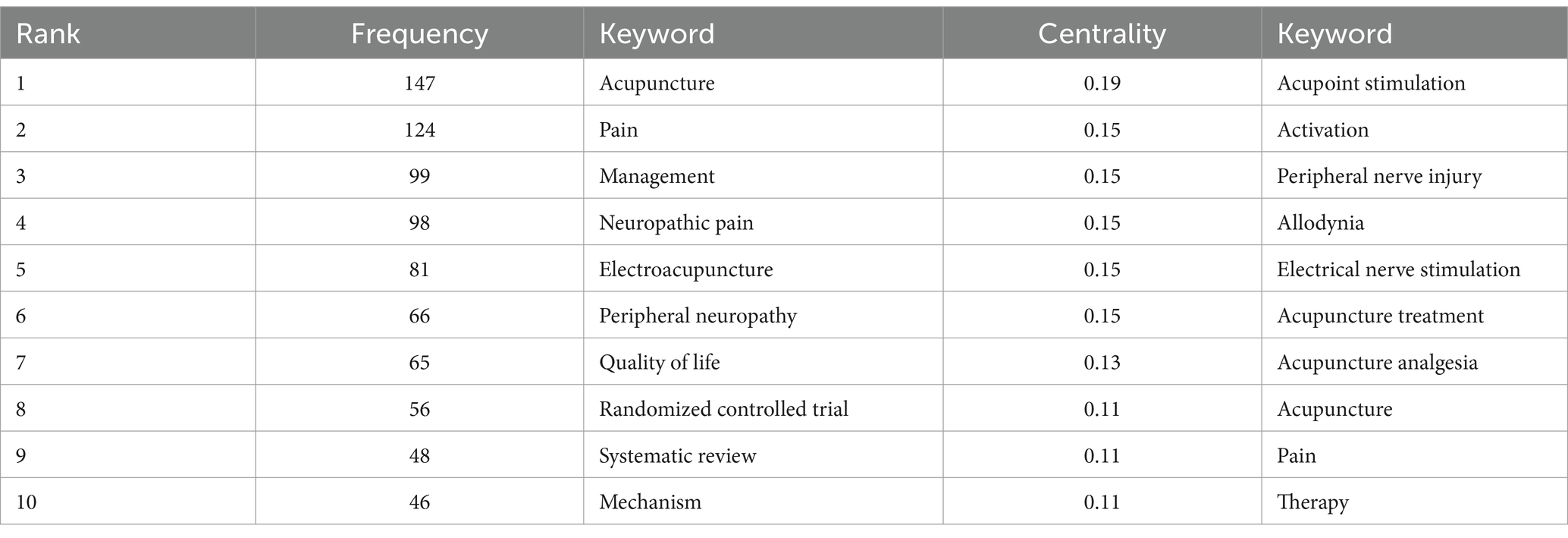
Table 2. The top 10 frequency and centrality of keywords related to acupuncture therapy for PNSD from 2004 to 2023.
In the study, burst words were identified as keywords that were frequently cited within a specific timeframe, underscoring emergent research areas. Figure 8A presents 25 keywords characterized by their initial year of prominence. Among these, “TN” emerged as the most potent, registering a peak strength of 4.32, although its prominence was brief, which lasting only one year. Conversely, “placebo-controlled trials” have demonstrated enduring relevance, originating earlier and sustaining their significance. At present, four keywords— “nerve,” “herpes zoster,” “safety,” and “traditional Chinese medicine”—continue to be identified as areas of ongoing research interest.
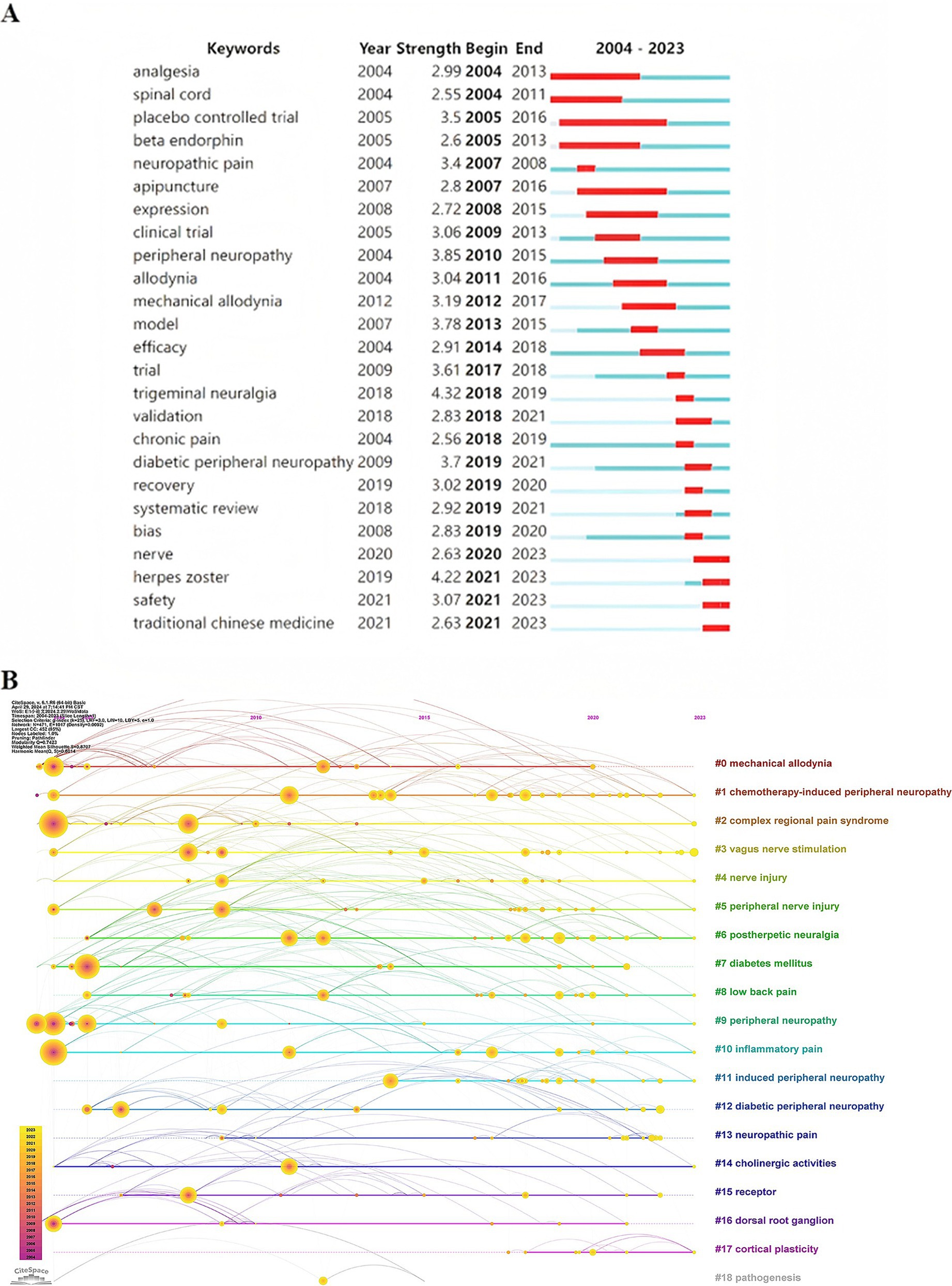
Figure 8. (A) Top 25 keywords with the strongest citation bursts. (B) Timeline view of keywords co-citation.
On the basis of the co-occurrence of keywords, they were clustered by the algorithm of CiteSpace, and 18 keyword cluster labels were obtained (Figure 8B). In this visualization, nodes represent keywords, arranged chronologically from left to right along the timeline at the top. Multicolored curves illustrate co-citation links between years, with larger nodes or nodes in warm colors signifying high citation frequency, citation bursts, or both. Clusters composed of homogeneous nodes are displayed vertically in descending order of size. Cluster #0, labeled “mechanical allodynia,” is the largest, containing 41 keywords, followed by “CIPN” (34 keywords), “complex regional pain syndrome” (31), “vagus nerve stimulation” (28), and “nerve injury” (28). Although Cluster #0 demonstrates the highest homogeneity, reflected by a silhouette score of 0.918, larger clusters generally exhibit slightly lower homogeneity than smaller clusters. Regarding cluster longevity, Cluster #0 spans 16 years and concludes in 2020, whereas Cluster #1 extends over 20 years and remains active through 2023, the most recent year analyzed.
3.2 Meta-analysis 3.2.1 Characteristics of the included RCTsA total of 7 RCTs related to acupuncture therapy for PNSD were included in this analysis (11, 27–32). All studies were published in English and involved a total of 489 patients, with 249 in the intervention group and 240 in the control group. The sample sizes ranged from a minimum of 32 to a maximum of 121 patients per study. Diagnostic criteria were not reported in one study, Ursini (28). Follow-up times were not reported in three studies: Kong (27), Gao (29), and Stringe (30), while the remaining studies provided this information. The basic characteristics of the included RCTs are summarized in Table 3.
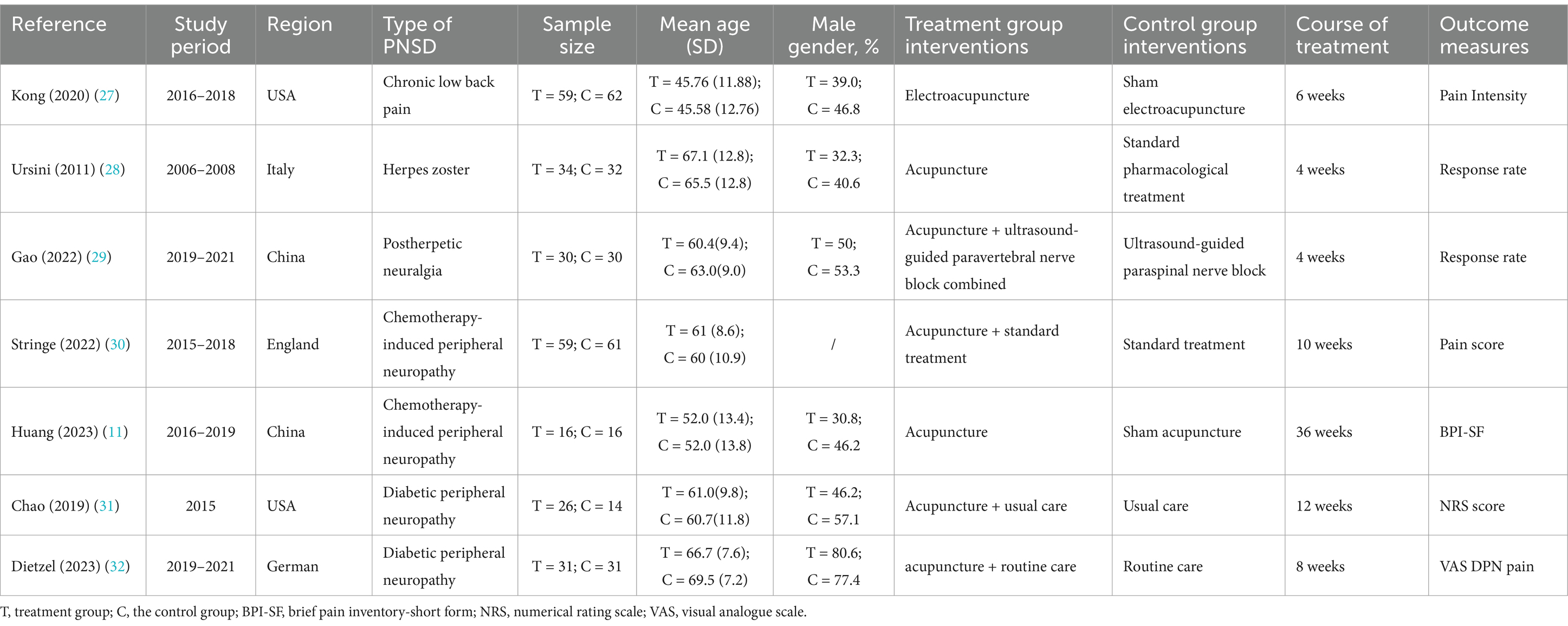
Table 3. The characteristics of included RCTs related to acupuncture therapy for PNSD from 2004 to 2023.
3.2.2 Quality assessment of the included RCTsThe risk of bias regarding the primary outcome across the 7 RCTs is detailed in Figure 9. Five RCTs utilized the random number table and computer software for sequence generation, indicating a low risk of bias (11, 27, 29, 31, 32). Two RCTs mentioned “random” without specifying details, resulting in an unclear risk of bias (28, 30). One RCT reported using opaque envelopes for sequence concealment (11), and another reported central randomization via telephone control (32), both of which were deemed to have a low risk of bias. Studies not providing this information were considered to have an unclear risk of bias. Two studies reported blinding methods: one applied blinding to patients and primary researchers without compromise (27), and the other employed blinding for participants, evaluators, and statisticians but not for acupuncturists and study coordinators, which was not deemed to introduce bias (11). Thus, the risk of bias for these studies was considered low. Studies not reporting blinding or not blinding both patients and primary researchers were considered to have an unclear or high risk of bias. All studies were assessed as having a low risk of bias regarding incomplete outcome data. Except for one study (27), the remaining RCTs did not report their study protocol. Since all studies had complete registration information and reported all expected outcome measures, including those pre-specified in the published literature, all RCTs were considered to have a low risk of bias. However, due to inadequate reporting on aspects such as random allocation methods, sequence concealment, and blinding implementation, along with a high risk of methodological bias, the overall methodological quality of the included RCTs was not considered high.
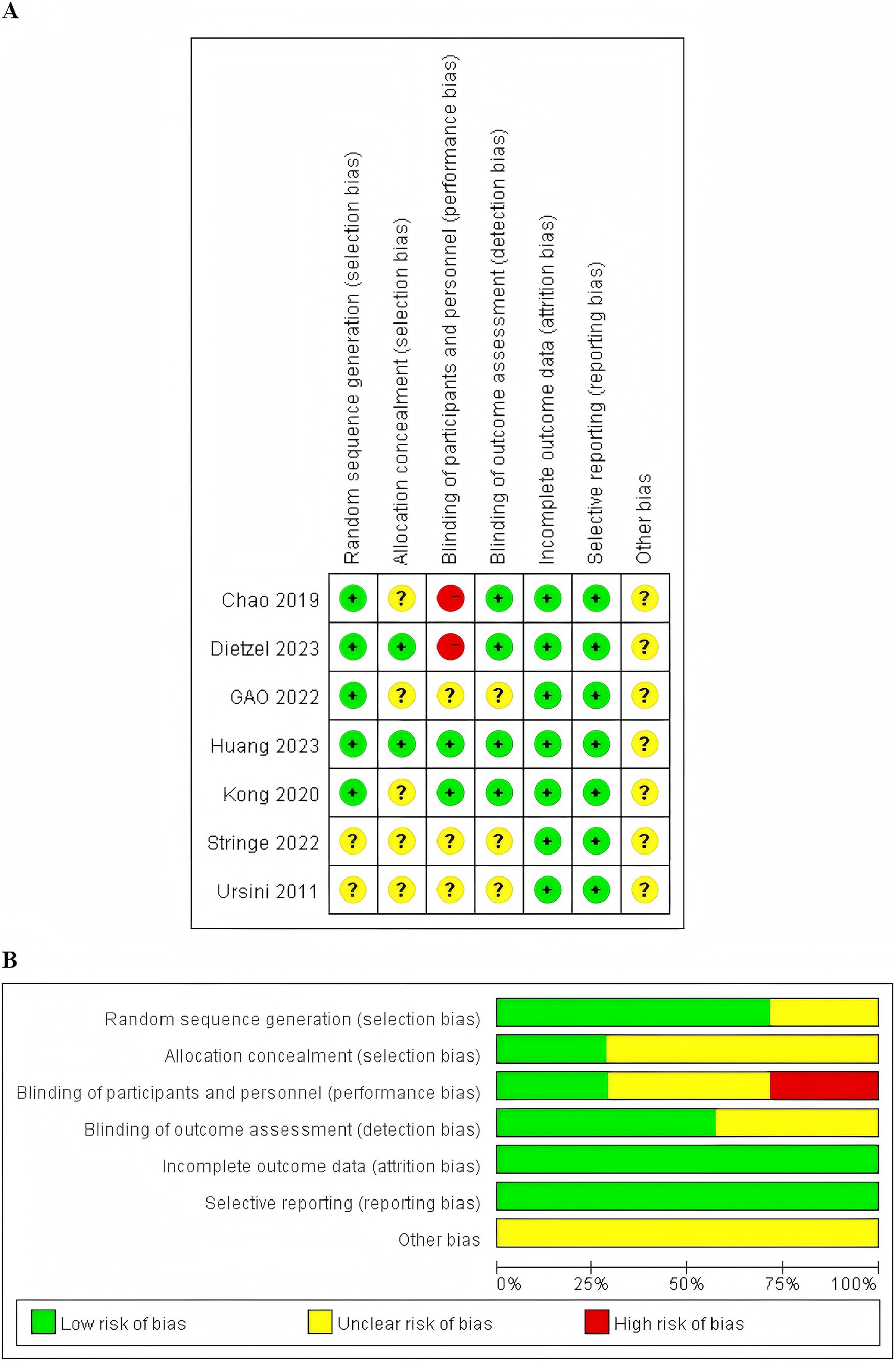
Figure 9. (A) Risk of bias of 7 included RCTs. (B) Risk of bias summary of 7 included RCTs.
3.2.3 Pain intensity of acupuncture for PNSDThe meta-analysis offers a comprehensive synthesis of the data, highlighting key trends and patterns observed across the included studies. The pooled effect sizes demonstrated that acupuncture significantly alleviated pain intensity associated with PNSD, with a mean difference (MD) of −1.18 (95% CI: −2.14, −0.23; p = 0.01) (Figure 10A). Heterogeneity was evaluated using the I2 statistic, revealing substantial variability. Subgroup analyses further examined potential moderators, providing insights into the heterogeneity of study characteristics, as outlined below.
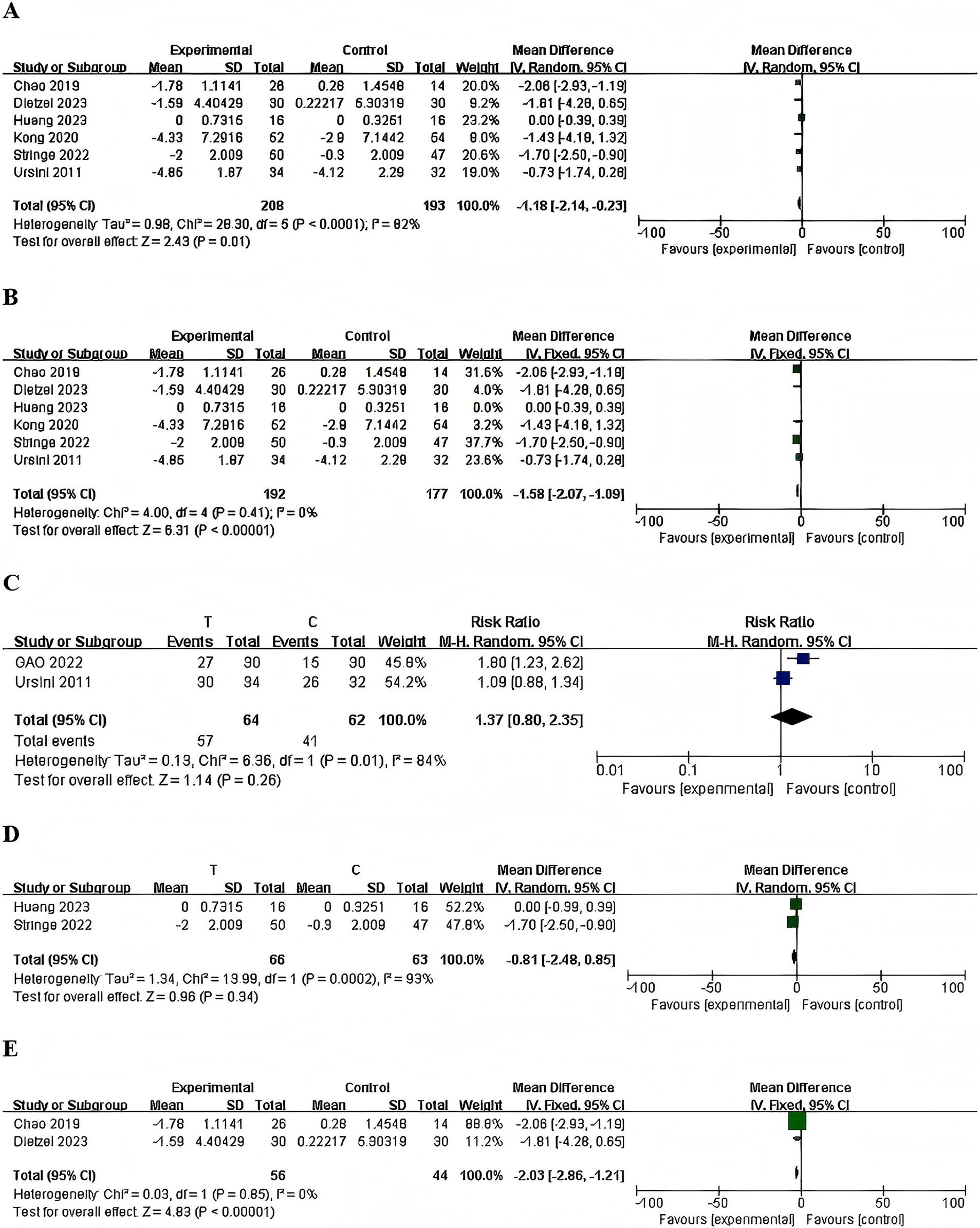
Figure 10. Forest plots of the pain intensity. (A) Total, (B) sensitivity analysis, (C) herpes zoster, (D) chemotherapy-induced peripheral neuropathy, (E) diabetic peripheral neuropathy.
3.2.3.1 Sensitivity analysisThe observed heterogeneity in the analyses can likely be attributed to variations in study designs, populations, and intervention protocols. To address this, we employed a Leave-One-Out Analysis, systematically excluding each study from the meta-analysis to evaluate its effect on the overall outcome. The sensitivity analysis identified a single study (11) as having a substantial impact on heterogeneity. Exclusion of this study led to a significant reduction in heterogeneity (I2), decreasing from 82 to 0%, indicating its central role in driving the observed variability. The pooled effect size remained robust (from p = 0.01 to p < 0.0001, with a new MD = −1.58, 95% CI [−2.07, −1.09]), reinforcing the stability of the analysis’ main conclusions, which are not contingent on the inclusion of this study (Figure 10B). These results prompted the exclusion of the study from the final analysis to enhance the reliability and interpretability of the findings.
3.2.3.2 Subgroup analysis 3.2.3.2.1 Chronic low back painOne RCT reported that electroacupuncture, compared with sham electroacupuncture, showed no significant difference in pain score changes (27). [MD = −1.43, 95% CI (−4.18, 1.32), one RCT, 106 participants, p = 0.31].
3.2.3.2.2 Herpes zosterThe random-effects model meta-analysis revealed no significant differences in herpetic zoster treatment outcomes between the acupuncture therapy group and the control group (28, 29). [RR =1.37, 95% CI (0.80, 2.35), 2 RCTs, 126 participants, p = 0.26] (Figure 10C).
3.2.3.2.3 Chemotherapy-induced peripheral neuropathyThe random-effects model meta-analysis indicated no significant differences in treatment outcomes between the acupuncture therapy group and the control group for CIPN (11, 30). [MD = −0.81, 95% CI (−2.48, 0.85), 2 RCTs, 152 participants, p = 0.34] (Figure 10D).
3.2.3.2.4 Diabetic peripheral neuropathyIn the comparison between acupuncture combined with usual care and usual care alone, the results indicated that acupuncture made significant difference in pain associated with Diabetic Peripheral Neuropathy (31, 32) [MD = −2.03, 95% CI (−2.86, −1.21), 2 RCTs, 102 participants, p < 0.0001] (Figure 10E).
3.2.4 Acupuncture safety, adverse eventsThe included studies exhibited considerable variation in the definition and monitoring of adverse events. Overall, acupuncture treatment was deemed safe, with no serious adverse events reported. One study documented 16 minor adverse events in 11 participants, including tingling, ache/pain, bruising, and minor bleeding, none of which required intervention or withdrawal from the trial (30). Another study reported a total of 43 adverse events associated with acupuncture out of 660 treatments administered; these included 18 small hematomas at single needling sites and seven instances of transient paraesthesia, with one case leading to a patient’s withdrawal from the intervention group (32).
3.2.5 Publication biasFunnel plots were generated to assess the potential for publication bias among the seven RCTs. The distribution of data points in the funnel plots appeared largely symmetrical (Figure 11).
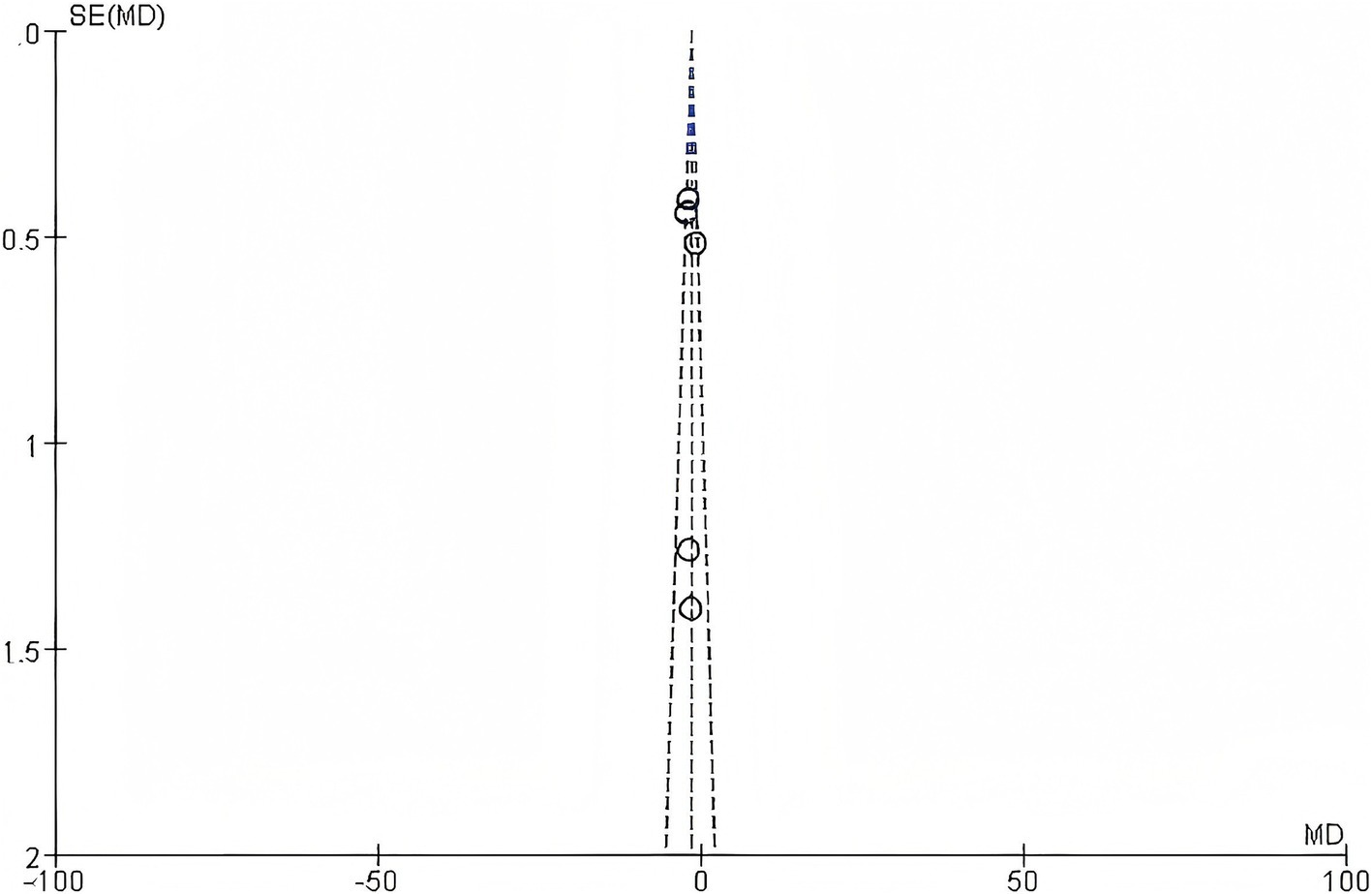
Figure 11. Funnel plot.
4 Discussion 4.1 General informationThis comprehensive bibliometric review illustrated a consistent uptick in the volume of publications on acupuncture therapy for PNSD spanning two decades. A marked increase in research output is evident starting around 2016, highlighting a growing interest in the therapeutic applications of acupuncture for PNSD in recent years. For the rising domestic incidence of PNSD (33), China, the United States, and South Korea emerged as principal contributors with notable publication outputs, contrasted by England, Italy, and Sweden, which demonstrated pivotal roles through their central positions in the literature network. Kyung Hee University, the China Academy of Chinese Medical Sciences, and Zhejiang Chinese Medical University were the leading institutions in terms of publication volume. Notably, Kyung Hee University was a pioneer in this field, initiating research as early as 2004. Although Zhejiang Chinese Medical University began its research efforts later, it has recently experienced a significant surge in literature output. Among individual researchers, Fang Jianqiao and Bao Ting were distinguished by their prolific contributions, yet the absence of centrality among authors suggested the lack of a stable collaborative network. A total of 71 research areas were identified among the publications included in this study. The top five most represented research areas are Integrative Complementary Medicine, Neurosciences, Medicine General Internal, Clinical Neurology, and Oncology. In terms of journal influence, “Pain” and “Anesthesia and Analgesia” stood out for their citation frequency and centrality, respectively, underscoring their influence in shaping the discourse within this field.
In current researches, meta-analyses and RCTs serve as the primary methodologies, focusing on the mechanisms and clinical implications of acupuncture. Over time, there has been a trend toward higher methodological rigor, including greater use of randomization, blinding, and standardized outcome measures. Nevertheless, the overall quality of extant research remains inadequate, with the evidence supporting the efficacy and safety of these interventions being limited. Significant challenges in this domain encompass small sample sizes, diverse study designs, and an absence of standardized protocols for acupuncture. Rigorous, large-scale RCTs are critical to delineate the specific benefits of acupuncture in both prophylaxis and treatment of PNSD.
4.2 Research hotspots 4.2.1 Acupuncture therapy in pain managementAcupuncture—a treatment with minimal side effects—has increasingly been adopted in global pain clinics for managing both acute and chronic pain scenarios. Extensive research corroborates its efficacy and safety in addressing diverse pain conditions (34–36). PNSD typically manifests with painful paresthesias, posing significant therapeutic challenges. Recent studies have rigorously assessed the therapeutic efficacy and safety of acupuncture in alleviating pain related to PNSD (37–40). Empirical data from multiple studies endorse acupuncture’s effectiveness in diminishing pain severity and minimizing functional disruptions, with minimal adverse events reported. Notably, clinical findings demonstrated that acupuncture not only diminishes pain across various time frames but also offers sustained pain management benefits (41, 42). Furthermore, emerging research underscored the potential of early acupuncture interventions to curb symptom progression and its synergistic benefits when combined with methylcobalamin in combating CIPN (24, 26).
Meanwhile, recent studies have provided mixed results regarding the efficacy of acupuncture for pain management. For instance, one investigation found no significant differences in pain relief between true acupuncture and sham groups at the 12-week mark (43). Similarly, another study is unable to confirm the benefits of acupuncture in reducing neuropathic pain or enhancing quality of life (44). The objective evaluation of acupuncture is inherently challenging due to the variability in practice techniques and the practitioner-dependent nature of treatment modalities. Furthermore, the effectiveness of acupuncture varies widely among different etiologies of PNSD (45, 46). The lack of a standardized placebo control also complicates the differentiation between placebo effects and treatment efficacy (47).
4.2.2 Acupuncture therapy for specific diseases 4.2.2.1 Chemotherapy-induced peripheral neuropathyResearch consistently highlights acupuncture’s efficacy in mitigating symptoms associated with CIPN, including significant reductions in neuropathic pain and paresthesia (24, 26, 48). Notably, RCTs have demonstrated marked improvements in sensory deficits, such as sensation loss and numbness (25). Observational studies further link these symptomatic improvements to enhanced nerve conduction, implying that acupuncture may promote nerve regeneration (49, 50). Importantly, significant enhancements in patient quality of life and reductions in neuropathy severity have been documented (51–53). Nevertheless, the efficacy of acupuncture varies due to differing methodologies, such as the choice between manual acupuncture (MA) and EA (54). Moreover, transcutaneous electrical nerve stimulation (TENS) has achieved notable pain relief in early treatment stages in a limited patient group, yet the intrinsic partially self-healing nature of CIPN necessitates further validation through rigorous RCTs (55).
4.2.2.2 Postherpetic neuralgiaPHN emerges as a chronic pain syndrome following herpes zoster infection, influenced by several risk factors including advanced age, immunosuppression, and autoimmune disorders such as systemic lupus erythematosus and diabetes mellitus, alongside recent physical trauma (56–58). Comprehensive research has established the efficacy of acupuncture in mitigating various forms of neuropathic pain, such as persistent spontaneous, paroxysmal, and mechanically evoked pain, the latter reflecting pathological amplifications of responses to both benign and noxious stimuli (59, 60). Beyond conventional acupuncture, alternative modalities exhibit distinct therapeutic indications and mechanisms, proving beneficial for PHN management. Notably, the use of filiform fire needle acupuncture coupled with mild moxibustion outperforms gabapentin in providing rapid analgesia, reducing pain swiftly with fewer side effects and at a lower cost. RCTs have demonstrated that combining EA at Jia Ji acupoints with moxibustion and intermediate frequency therapy effectively alleviates pain and anxiety in PHN sufferers. Additionally, evidence supports the effectiveness of collateral-pricking and bloodletting cupping combined with EA in enhancing pain relief, sleep quality, and overall therapeutic outcomes in PHN patients (61).
4.2.2.3 Trigeminal neuralgiaAcupuncture is increasingly recognized as a therapeutic intervention for TN. Empirical evidence underscores its role in mitigating the distinctive, severe pain often described as intermittent, electric shock-like sensations affecting the trigeminal nerve divisions (62, 63). A longitudinal analysis supports acupuncture’s therapeutic potential, particularly its analgesic benefits for TN and associated myofascial pain (64). Moreover, clinical trials have documented enhancements in cognitive function and overall quality of life for patients undergoing acupuncture treatment for this neuralgia (65). Additionally, meta-analytical findings suggest that acupuncture provides beneficial effects in managing persistent TN with a favorable safety profile, although the evidence is limited by the methodological shortcomings of the included RCTs (42).
4.3 Research frontiers 4.3.1 Focus on patient-reported outcomesPatient-reported outcomes, such as reductions in pain and improvements in quality of life, were consistently documented across numerous studies, emphasizing the therapeutic potential of acupuncture. Future research should prioritize the development of personalized approaches by aligning treatment protocols with individual symptomatology, pain severity, and patient preferences. The integration of pharmacological and non-pharmacological strategies—including acupuncture, moxibustion, and electroacupuncture—offers a promising avenue to optimize clinical outcomes and advance holistic care paradigms (59, 60).
Besides, there is an urgent need for studies that elucidate the precise mechanisms by which acupuncture modulates PNSD. Determining whether the observed benefits are attributable to the acupuncture itself, placebo effects, or a combination thereof is crucial. Despite the ongoing debate surrounding its placebo effects, current evidence does not justify excluding acupuncture as a treatment option under suitable conditions, particularly considering accessibility and cost factors (66).
4.3.2 Cost-effectiveness analysisEconomic evaluation, particularly cost-effectiveness analysis (CEA), is an essential yet often underappreciated aspect of assessing the feasibility of integrating acupuncture interventions into clinical practice. Such evaluations involve analyzing therapeutic benefits and patient outcomes in relation to the associated costs. Incorporating CEA into acupuncture research provides a more comprehensive understanding of the practicality and economic viability of acupuncture across diverse healthcare settings. For example, CEA can help determine whether acupuncture is a cost-effective alternative to conventional treatments in primary care or if it offers value for money in specialized pain management clinics (67, 68). These insights are crucial for informing policy development, clinical practice guidelines, and for guiding both patients and healthcare providers toward the most appropriate and cost-effective treatment options. The feasibility of conducting CEA in acupuncture research is well-established. Several studies have successfully applied economic evaluation methods to acupuncture interventions (69, 70). While this study does not include a cost-effectiveness analysis, we recognize its importance and recommend that future research incorporate economic evaluations to assess the feasibility of acupuncture in various healthcare environments.
Additionally, research funding is a key determinant in guiding academic inquiry and driving innovation. Our analysis observed a predominance of government-sponsored projects, with limited insight into the role of private organizations due to data constraints. This gap underscores the importance of developing more robust datasets that encompass the range of funding sources. Subsequent studies should prioritize the collection of such data to elucidate how funding patterns influence the therapeutic strategies.
4.3.3 Implications for future researchAcupuncture is a globally practiced therapy, and the increased funding for clinical acupuncture studies has facilitated the generation of high-quality primary clinical evidence (71). This study employs CiteSpace visualization software to objectively examine key trends in acupuncture therapy for PNSD from 2004 to 2023. By integrating recent advancements in the field, we aim to delineate the underlying factors that shape research trajectories.
To ensure data consistency and quality, only English-language publications were included in this analysis. However, this approach may introduce language bias by excluding potentially relevant studies published in other languages. Future research should incorporate studies from diverse linguistic sources to mitigate this bias. Moreover, the small sample sizes and significant variations in research designs across current studies highlight the urgent need for large-scale, high-quality RCTs and systematic evaluations. Future studies should seek to enhance the number of RCTs by refining inclusion criteria and conducting additional rigorous trials. Furthermore, a notable limitation of this review lies in the methodological heterogeneity of acupuncture interventions across included studies. Critical parameters such as acupoint selection rationale, needling techniques, and treatment duration were inconsistently reported, preventing subgroup analyses to disentangle their effects. This reflects a broader challenge in acupuncture research, where personalized protocols often prioritize clinical flexibility over standardization. Future research endeavors should concentrate on ameliorating methodological limitations by implementing stringent blinding of subjects and investigators, standardizing acupuncture techniques, and adopting validated, objective evaluation metrics (72). Evaluating the long-term efficacy of acupuncture relative to established pharmacological therapies (73), and investigating the optimal frequencies and combinations of acupuncture interventions are paramount (74–76).
Additionally, with an enhanced understanding of the various types and specific symptoms of PNSD, future research could increasingly focus on the efficacy of acupuncture in addressing sensory impairments (e.g., numbness, paresthesia) and improving quality of life outcomes. Subsequently, further explorations into the specific mechanisms and therapeutic effects of MA, EA, moxibustion, and other alternative therapies, are warranted. Lastly, with the advancement of precision medicine and personalized treatment approaches, future research should focus on customizing treatment plans to the specif
Comments (0)