People who inject drugs (PWID) in India, like those in other parts of the world, have a disproportionately high HIV burden. Several large-scale studies, including those conducted by the Indian government, have documented a high HIV prevalence of 9 to 18.1 per cent1,2 among PWID, about 30 to 70 times higher than that among the general population (0.21%)3, and a high HIV incidence of 2.9 per 100 person-years2. In the past few years, HIV prevalence among PWID has been increasing in certain regions, especially the northern parts of India1. The National AIDS Control Organisation (NACO) has supported targeted HIV interventions among PWID for the past decade. These interventions have focused on HIV awareness/education, needle/syringe distribution and exchange, opioid substitution treatment (buprenorphine), and condom distribution4. Knowledge about HIV and syringe/needle sharing as a mode of HIV transmission is reportedly high among PWID. For example, >90 per cent of PWID reportedly have correct knowledge about three routes of HIV transmission, and 88 per cent have reported knowing that avoiding needle/syringe sharing can prevent HIV transmission1. Despite this knowledge, needle/syringe sharing among PWID remains quite high. Accordingly, HIV prevalence among PWID has remained constant over the past decade, in comparison to HIV prevalence in other key populations (like female sex workers)4.
Syndemics theory proposes that diseases or negative health outcomes cluster and concentrate in certain populations or settings due to detrimental social conditions, as they mutually reinforce and synergistically intensify the burden of disease5. In the context of HIV among PWID, experiences like incarceration or violence victimisation and behaviours like needle/syringe sharing can be viewed as components of a syndemic as these not only cluster together due to shared social and structural determinants (e.g., social marginalization) but may also interact to amplify HIV risk beyond their individual effects. The syndemic of substance abuse, violence victimisation, and HIV was one of the first to be described5. Among PWID, other syndemic exposures that have been documented or proposed include depression6,7, incarceration experience8, violence victimisation6, intimate partner violence7, and viral hepatitis8,9. In India, syndemics of non-communicable diseases are being increasingly reported while those on communicable diseases lag behind, becoming important10,11, thus, highlighting the need to study non-communicable syndemic conditions such as violence victimisation and incarceration.
HIV epidemic among PWID in India must be viewed in certain socio-structural contexts, such as stringent laws against the use of drugs, negative societal attitudes towards people who use drugs, and discrimination faced by PWID in families and healthcare settings12,13. Research on the co-occurrence and synergistic interactions of health risks among PWID in India remains scarce. Investigating these synergies is crucial for both theoretical understanding and practical application14.
Studies from India have shown that PWID are at a high risk of being arrested for drug-related offences12,15. Several possible mechanisms could explain how incarceration increases HIV acquisition or transmission among PWID: access to injection drugs, lack of access to clean needles/syringes during incarceration16; potential increases in substance use, needle/syringe sharing, inconsistent condom use, and/or transactional sex during incarceration or after release17,18; and lack of employment opportunities and suboptimal mental health for persons with a history of incarceration17,19.
While violence perpetrated by PWID has been reported to be a reason for the elevated arrest rates16, PWID also faces high rates of physical violence from family members, strangers, police, and other PWID12,15. Fear of arrest and violence from police and others may prevent PWID from carrying clean needles/syringes, resulting in elevated rates of needle/syringe sharing among PWID15, and may also prevent PWID from accessing health care services, including syringe exchange programmes12. Finally, it is possible that poor mental health secondary to discrimination and experience of violence may undermine agency and self-efficacy, preventing PWID from adopting safer injecting practices20.
Systematic reviews by Tsai and Burns14, and Tsai et al21 showed that most papers claiming to have tested the syndemic theory have not used suitable analytical methods. Most studies included the number of exposures as a cumulative count to predict HIV risk, which is not compatible with the interaction concept rooted in syndemic theory22. Although two recent large-scale studies among men who have sex with men from India appropriately assessed the relative excess risk due to interaction from adjusted regression models23,24, as per our knowledge no studies from India or other lower- and middle-income countries have studied syndemics among PWID using appropriate statistical methods.
How diseases interact at the individual level, or how epidemics interact at the population level, have been described by several theories of disease distribution25, based on which Tsai proposed three potential ways in which the relations between co-occurring epidemics can be conceptualised: mutually causal epidemics, synergistically interacting epidemics, and serially causal epidemics. The former two, although different in terms of statistical conceptualisation, have often been used interchangeably in syndemics literature. The third model is also statistically distinct from the other two but, on occasion, has been interpreted as being consistent with the original conceptualisation of syndemics26.
To fill these knowledge gaps, this study was undertaken to analyse data from a population-based study from India conducted among men who inject drugs to test two of the three models of co-occurring epidemics described by Tsai25: (i) the model of synergistically interacting epidemics, in which the joint associations between HIV and incarceration experience, physical violence victimisation and needle/syringe sharing were evaluated, and assessed for synergistic interaction using both additive and multiplicative scales; and (ii) the chains of risk model27, in which needle/syringe sharing was conceptualized as a potential mediator of the effect of incarceration experience and violence victimisation on the HIV status.
Materials & MethodsThis was a secondary analysis of data obtained from a population-based, cross-sectional survey conducted during 2014/15 among men who inject drugs as part of the NACO’s Integrated Bio-Behavioural Surveillance (IBBS) study1, which aimed to better understand HIV risk behaviours among key populations, with the goal of informing intervention efforts.
ParticipantsUnder the IBBS 2014-15 survey, a total sample of 19,902 men who inject drugs were enrolled and analysed across 53 domains in 29 States and Union Territories in India, with a 90 per cent response rate. ‘Men who inject drugs’ in this survey were defined as men, aged ≥ 15 yr, who had used any psychotropic (addictive/mind-altering) substance or drug for recreational or non-medical reason through injections, at least once in the past three months.
Survey unit and samplingThe IBBS survey unit was a domain, which could either be a single district or a group of districts sharing similar socio-cultural norms. Domains were selected randomly, and the required sample size for a potential domain was about 400, based on the following criteria: a 50 per cent baseline value for condom use with a paid partner, ability to detect a 15 per cent change between survey rounds, 0.05 alpha level, 90 per cent power, and a 1.7 design effect1.Time-location cluster sampling was used. Time-location clusters refer to sites such as parks and abandoned places where men who inject drugs might be found on particular days and times, or where they congregate with other PWID. Temporary private venues were established near time-location clusters to collect blood specimens using the dried blood spot (DBS) method and tested for HIV in 16 labs across India. All samples testing positive, and two per cent of those testing negative, were re-tested at the ICMR-National AIDS Research Institute, Pune.
Measures of exposure Primary exposures of interest Incarceration experienceParticipants were asked if they had ever been to prison for any activities related to drug use in last 12 months. Those who reported ‘yes’ were categorised as having ‘any incarceration experience’.
Violence victimizationParticipants were asked about the frequency of physical violence endured over the past year, defined as being hurt, hit, slapped, pushed, kicked, punched, choked, or burned. Two categories were created: ‘any violence victimisation’ for any reported incident, and ‘severe physical violence victimisation’ for six or more incidents.
Needle/syringe sharingTwo questions were asked pertaining to whether the participant lent or borrowed used needle/syringe from a fellow user. The responses were dichotomised into ‘yes’ or ‘no’, and a single variable ‘needle/syringe sharing’ was then created by combining the responses to those two questions.
Outcome measuresThe outcome measure was HIV-positive status as determined by testing DBS specimens collected from participants using two different Enzyme-Linked ImmunoSorbent Assay (ELISA) kits (Microlisa HIV, J. Mitra & Co. Pvt. Ltd., New Delhi and SD Bioline HIV-1/2 3.0, New Delhi, Alere Medical Pvt. Ltd., Gurgaon). The apex laboratory at ICMR-National AIDS Research Institute validated and distributed these kits to testing labs.
Covariates Sociodemographic and related characteristicsDemographic variables included age (in years), educational attainment, and marital status.
Inconsistent condom use with non-regular partnersAs the probability of secondary HIV transmission per coital act is reportedly higher for receptive peno-vaginal intercourse compared with insertive peno-vaginal intercourse28, we developed a dichotomous variable where inconsistent condom use with either male casual partners or female paid partners was coded as ‘1,’ otherwise ‘zero.’ By including inconsistent condom use as a covariate, the adjusted effect of the exposure variables could then be determined, given that both inconsistent condom use and needle/syringe sharing contribute to HIV risk.
HIV risk knowledgeParticipants were evaluated on their understanding of four HIV transmission routes (condomless sex, needle sharing, blood transfusions, and vertical transmission) and one misconception (transmission via mosquito bites). Correct responses were assigned a value of 1, while incorrect answers received 0.
HIV programme exposureHIV intervention exposure (in the previous year) was measured by participants’ self-reported involvement with 10 HIV-related services (e.g., HIV/STI education, distribution of condoms) offered by non-governmental organisations. The totals core ranged from 0 to 10.
AnalysisThe analyses followed directly from the conceptual considerations reviewed above, but the specific analytic plan was not preregistered. Given the complex survey design, we used the svyset command in Stata29. No data were missing for HIV status or needle/syringe sharing. The exposures of violence victimisation and incarceration variables had 0.06 per cent and 1.91 per cent missingness, respectively. Given the small percentage of missing data, case-wise deletion was used.
To examine the model of synergistically interacting epidemics, we included product terms in the regression models to assess for two- and three-way interactions. This was done on both the additive and multiplicative scales30, between three key variables, namely, past-year violence victimisation (yes/no), past-year incarceration experience (yes/no), and needle/syringe sharing during the previous episode of injection drug use (yes/no). The dichotomous outcome measure was HIV-positive status (yes/no). Regression models included covariates such as age, education, marital status, inconsistent condom use, HIV knowledge, and HIV programme exposure (Supplementary material 1).
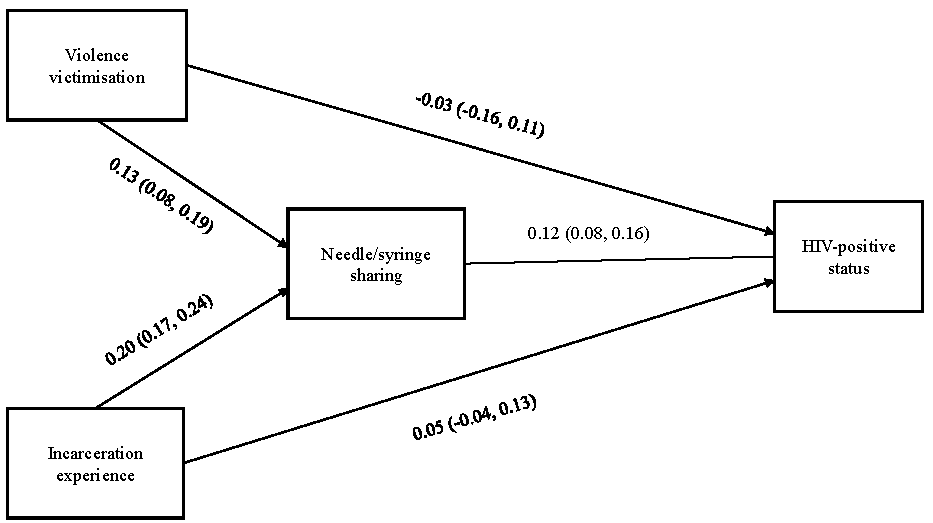
To evaluate the model of serially causal epidemics, we conducted a mediation (path model) analysis (Figure) using MPlus (version 7.2)31. For this analysis, we specified needle/syringe sharing as a continuous variable ranging from 0 to 2, and the other two exposure variables (incarceration experience and severe violence victimisation) and the outcome variable (HIV status) as binary measures. Given that incarceration experience and violence victimisation are associated with HIV risk8,12,19, we tested the extent to which the associations between incarceration experience and HIV status, and between violence victimisation and HIV status, were mediated through needle/syringe sharing. We estimated the bias-corrected confidence intervals of the direct, indirect, and total effects with 2000 bootstrap samples.
Export to PPT
ResultsThe participants’ median age in this study was 29 yr, 45.6 per cent were currently married, and the median of education was standard 9 (range: 0 to 16) (Supplementary Table I). The weighted average national HIV prevalence among men who inject drugs was 9.9 per cent [95% confidence interval (CI), 9.0% to 10.9%]. Past-year incarceration was reported by 1,998 (10.2%) participants; among them, 568 (28.4%) reported having injected drugs within prisons, consistent with available knowledge about how drugs are readily accessible within prisons17,22. Physical violence was reported by 6,915 (34.7%) participants. Among these, the reported violence was perpetrated by family members (40%; 2,766), strangers (33.1%; 2,351), fellow men who inject drugs (28.2%; 1,954), police (13.0%; 901), and goondas (thugs) (11.4%; 686).
Co-occurrence of adverse exposuresAmong the 19,902 men who inject drugs, incarceration experience (n=1,998; 10.2%), any violence victimisation (n =6,915; 28.4%), and needle/syringe sharing (n=3,542; 17.8%) frequently co-occurred: 799 (4%) reported both violence victimisation and incarceration, 1290 (6.5%) reported both violence victimisation and needle/syringe sharing, 213 (1.1%) reported incarceration and needle/syringe sharing, and 387 (1.9%) reported all three exposures. Fifty-two per cent of the participants reported no adverse exposures (n=10528; 52.9%). When violence exposure was limited to severe physical violence victimisation (as in the subsequent analyses), then only 0.3 per cent reported all three exposures.
Model of synergistically interacting epidemicsIn a logistic regression model with no interaction (cross-product) terms, needle/syringe sharing [Adjusted odds ratio (aOR)=1.33, 95% CI, 1.08 to 1.63] was significantly associated with HIV-positive status, but not with violence victimisation (aOR=0.8, 95% CI, 0.56 to 1.13) and incarceration (aOR=1.18, 95% CI, 0.88 to 1.59). Synergy between epidemics was assessed by incorporating interaction terms in the logistic regression models. To maintain uniformity in model comparison, three separate logistic regression models (Models 1, 2, and 3 in Table) were built, with each model having a single two-way interaction term. In a logistic regression model with all three two-way product terms (Model 4 in Table), a significant two-way multiplicative interaction between violence victimisation and needle/syringe sharing were found (Semi-elasticity=0.65, 95% CI, 0.01 to 1.29), which means that the joint effect of these two exposures, above and beyond their individual associations with HIV-positive status, was associated with a 65.5 per cent point increase in the outcome. We then fitted a logistic regression model with all three two-way product terms and the three-way product terms (Model 5 in Table). In this model, we estimated a statistically significant three-way multiplicative interaction between incarceration, violence victimisation, and needle/syringe sharing. The joint effect of these three exposures, above and beyond individual associations with HIV-positive status, was associated with a 186.1 per cent point increase in the outcome (Semi-elasticity=1.86, 95% CI, 0.51 to 3.20).
Table. Effects of interacting adverse psychosocial exposures on the multiplicative scale (N=19,902)
Model 1: Two-way interaction term (V x I) Model 2: Two-way interaction term (V & S) Model 3: Two-way interaction term (I & S) Model 4: All two-way interaction terms Model 5: All two- and three-way interaction termsEstimated
semi-elasticity
(95% CI), P value
Estimated
semi-elasticity
(95% CI), P value
Estimated
semi-elasticity
(95% CI), P value
Estimated
semi-elasticity
(95% CI), P value
Estimated
semi-elasticity
(95% CI), P value
V x I 0.32 (-0.4, 1.05), P=0.37 0.31 (-0.38, 1.02), P=0.37 -0.66 (-1.59, 0.25), P=0.15 V x S 0.63 (-0.02, 1.28), P=0.05 0.65 (0.01, 1.29), P=0.04 0.13 (-0.57, 0.84), P= 0.71 I x S -.28 (-0.83, 0.25), P=0.3 -0.33 (-0.86, .19), P=0.21 -.48 (-1.04, .07), P=0.09 V x I x S 1.86 (0.51, 3.20), P=0.007Among the other covariates included in the fully saturated multivariable logistic regression model, higher odds of HIV-positive status were estimated for participants who were currently single (aOR=1.35, 95% CI, 1.12 to 1.62) and for older-age participants (aOR=1.02 per year, 95% CI 1.01 to 1.03). Lower odds of HIV-positive status were estimated for participants with fewer years of education (aOR=0.89 per year, 95% CI, 0.87 to 0.9). In a sensitivity analysis specifying violence victimisation and needle/syringe sharing as continuous variables; we obtained qualitatively similar findings.
In the linear probability regression models to estimate the relative excess risk of interaction (RERI), we found no evidence for additive interaction in the models that included the main effects and one two-way product term at a time (Models 1, 2 and 3 in Supplementary Table II) and all three two-way product terms (Model 4 in Supplementary Table II). However, in the fully saturated linear probability regression model, the three exposures of interest had a synergistic interaction (RERI=0.21, 95% CI, 0.03 to 0.38, P=0.02) (Model 5 in Supplementary Table II). This non-zero, positive, and significant estimate indicates that the RERI exceeds 0.
Model of serially causal epidemicsIncarceration had a significant indirect effect (0.02, 95% CI, 0.01 to 0.03) on HIV-positive status, but direct (0.04, 95% CI, -0.03 to 0.12) and total effects (0.07, 95% CI, -0.01 to 0.15) were not significant (Figure). Similarly, we found a significant indirect (0.01, 95% CI, 0.008 to 0.025) effect of severe violence victimisation on HIV-positive status, but the direct (-0.02, 95% CI, -0.17 to 0.09) and total (-0.01, 95% CI, -0.15 to 0.11) effects were not significant. Taken together, these findings provide partial support for the mediation model.
DiscussionUsing a probability-based cross-sectional survey data of 19,902 men who inject drugs in India, it was found that incarceration experience, violence victimisation, and needle/syringe sharing frequently co-occurred, and that needle/syringe sharing had a robust, a significant association with the HIV-positive status. We assessed two models of co-occurring epidemics25, namely, synergistically interacting epidemics model, in which the combined effects of incarceration experience, severe violence victimisation, and needle/syringe sharing on HIV status were examined on both the additive as well as multiplicative scales, and a serially causal epidemics model, in which needle/syringe sharing was tested as a potential mediator of the effect of both incarceration experience as well as severe violence victimisation. On both multiplicative as well as additive scales, evidence for a synergistic three-way interaction between incarceration experience, severe violence victimisation, and needle/syringe sharing was found. However, on the multiplicative scale, evidence of synergistic two-way interactions between severe violence victimisation, and needle/syringe sharing was found. It is important to note that while this subgroup of individuals subjected to all three exposures should be considered extremely vulnerable, this subgroup represented only 0.3 per cent of all men who inject drugs sampled in the study. In testing the model of serially causal epidemics, the significant indirect effects of both incarceration experience and severe violence victimisation on HIV status through needle/syringe sharing were estimated. However, there were no significant direct or total effects of incarceration or violence victimisation on HIV status. Thus, the evidence of synergistically interacting epidemics model was strong but less strong for the model of serially causal epidemics.
The synergistic interactions between incarceration experience, violence victimisation, and needle/syringe sharing found in this study are consistent with existing research18. Studies from India have shown that injection drug use is prevalent within prisons, where clean needles/syringes are lacking, which may facilitate needle/syringe sharing16,19 and, in turn, increase the risk of HIV infection9. The World Health Organization recommends a package of interventions, including needle/syringe programmes in prisons and in other closed settings32. Recently, NACO has begun to support HIV prevention intervention projects in prisons, but without needle/syringe exchange programmes33,34. As noted earlier, physical violence victimisation may increase the risk for HIV infection by decreasing psychological well-being and/or the ability to protect oneself from infection, in turn leading to needle/syringe sharing and restricted access to HIV prevention and treatment services15,19. Most studies of interpersonal violence have focused on the role of intimate partner violence and sexual violence on HIV-related risk behaviours35. Given the lack of specific data on sexual violence against men who inject drugs in this dataset, we could not include sexual violence as part of the violence victimisation exposure variable.
Most studies exploring syndemics among PWID have assessed depression6,7, intimate partner violence (particularly among women who use drugs)7, sexual risk behaviours7, and needle/syringe sharing36 as exposures or outcomes. None of the studies of syndemics among PWID have focused directly on incarceration experience and HIV infection. Further, only a few studies among PWID have used appropriate statistical methods for assessing synergism36. None have tested multiple models of co-occurring risks.
Our study has several limitations and strengths that warrant consideration (Supplementary material 2). Key limitations include the cross-sectional design precluding causal inferences, potential underreporting of incarceration due to social desirability bias, inability to directly compare non-nested models, and exclusion of women who inject drugs. Notable strengths include being the largest probability-based syndemic study among PWID to date and the use of appropriate statistical methods for assessing interactions. Despite using 2014/15 data, this study remains relevant by providing a baseline for understanding syndemic processes among PWID in India and identifying key gaps that persist in current interventions.
The study findings indicate that needle/syringe sharing independently, and in concert with incarceration experience and violence victimisation synergistically, increases the risk of HIV infection. This suggests that interventions targeting even one or two of these three exposures could potentially reduce HIV risk. However, integrated, multicomponent interventions addressing all these exposures, given the interconnections between these three exposures (as revealed in the serially causal model), could be more effective in reducing HIV risk. For exposures that lead to other exposures (e.g., incarceration leading to needle/syringe sharing), multi-level interventions might be more effective. For example, at the prison level - HIV prevention and substance use prevention and care interventions, such as screening and treatment of substance use disorders, provision of clean needles/syringes, naloxone for overdose, opioid substitution therapy, post-release employment, and mental health support, and actively linking recently-released men who inject drugs with HIV prevention services8; and at the individual level - screening and management of violence victimisation or its mental health consequences.
Overall, our research provides empirical evidence to suggest that there is a syndemic of violence victimization, incarceration experience, and needle/syringe sharing among men who inject drugs in India that amplifies their risk of HIV. Synergistic (additive and multiplicative) interactions were found between violence victimisation, incarceration experience, and needle/syringe sharing on HIV-positive status. Evidence for the model of serially causal epidemics suggests that preventing violence victimisation could potentially reduce needle/syringe sharing, thereby decreasing HIV transmission. Future studies should focus on gathering empirical evidence demonstrating the extent to which large-scale social and structural forces give rise to syndemics. These studies could adopt longitudinal mixed methods approaches and employ multi-level analyses, to elucidate interactions between various adverse psychosocial exposures. Such an understanding of the production and nature of syndemics will further contribute to both theory and program design and implementation.
Comments (0)